During the September 2021 Maternal Mental Health Technical Consultation, a speaker recalled how her family fled during the Rwandan genocide and the toll it had on her mother’s mental health. As the head of the family, her mother bore the brunt of the emotional responsibility of that traumatic experience. She remembers a period growing up where her mother “went to a place where we couldn’t reach her.” She was experiencing depression and found it difficult to access the care she needed while her family was living as refugees. This had an adverse impact on her and her family as they watched their mother struggle.
The story of this mother and her family is just one example of how we must meet mothers where they are when it comes to maternal mental health. Nearly one billion people around the world live with a mental health condition and of those, 90% live without treatment..1 Despite being recognized as a fundamental aspect of overall health and as one of the Sustainable Development Goals (SDGs) by the World Health Organization (WHO), mental health remains underfunded and often ignored. Maternal mental health encompasses the health and wellness of women during pregnancy, childbirth, and the postnatal period. Approximately one in five women experience depression during pregnancy and in the first three months of postpartum.2 Up to 20% of mothers with perinatal mental health conditions experience suicidal thoughts.3 And the effects extend beyond self-harm; the mental health of a mother has a direct impact on the wellbeing of her children and the entire extended family. Moreover, the COVID-19 pandemic has dramatically increased the need for mental health support worldwide, especially for new and expectant mothers.
While all mothers deserve mental health support during the perinatal period, mothers in fragile and crises-affected contexts in particular experience poorer maternal mental health outcomes and higher rates of Common Perinatal Mental Disorders (CPMDs). People living through conflict, crisis or emergency endure multiple hardships, both physical and emotional. For many women, whether already a mother or an expectant mother, the weight of familial responsibility adds to that emotional burden.
“Maternal mental health is not a luxury; all women deserve maternal mental health. It is a basic and fundamental human right and is central to human dignity.”
Paul Bolton
USAID MHPSS Coordinator
In an effort to document the gaps in services, data, resources, and overall attention to maternal mental health globally, USAID’s MOMENTUM Country and Global Leadership (MCGL) Project, in collaboration with WHO and UNFPA, undertook a global scoping exercise that held focus group discussions with humanitarian and development experts, explored recent research and literature, and noted various key recommendations for maternal mental health. These findings and recommendations were published in a brief: The Silent Burden: A Landscape Analysis of Common Perinatal Mental Disorders in Low- and Middle-Income Countries. Simultaneously, a three-day Maternal Mental Health Technical Consultation was organized to discuss and review the findings. The consultation brought together 900 experts representing 89 countries from across the humanitarian-development nexus. Important topics were covered such as: Approaches for Integration of Maternal Mental Health Care in Fragile and Affected Contexts; Integrating Maternal Mental Health into Existing Small and Sick Newborn and Nutrition Interventions; Linkages between Respectful Maternity Care (RMC) and Maternal Mental Health Movements; and Reducing Maternal Mental Health Stigma – to name a few.
As a member of the humanitarian community, I was encouraged by the consistent emphasis placed by speakers and presenters alike on the mental health of mothers in the most vulnerable situations. The technical consultation featured two sessions dedicated to maternal mental health in fragile and crisis-affected settings: one summarized the current evidence and gaps in maternal mental health and the other highlighted approaches to maternal mental health with a focus on integrated service delivery.
In the first session focused on the evidence and gaps, speakers (Isabella Ochieng – MCGL, Lincoln Ndogoni – Psychosocial Support Centre, Dr. Laura Murray -JHSPH) stressed that in a crisis, health systems are often not well positioned to manage perinatal mental health problems, and follow up and support can be particularly challenging with migrant populations. Country implementers noted that mothers often identify their mental health challenges using their own language or idioms that often do not fit clinical diagnosis. “Interventions must respond to how mothers identify their mental health struggles and experiences.”4 Speakers called for an increase in research priorities relevant to the conditions most prevalent in humanitarian settings, saying that “sometimes the research done responds to the researcher’s needs, rather than the individual’s needs.”5
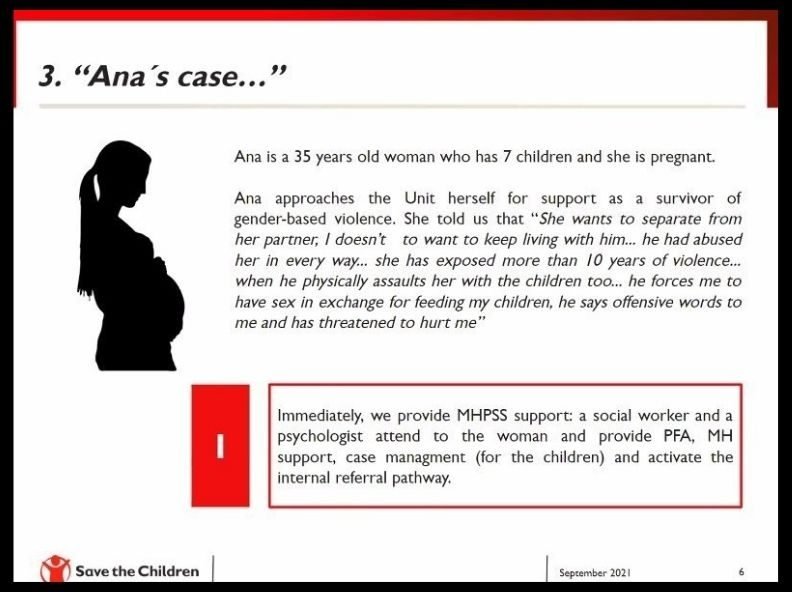
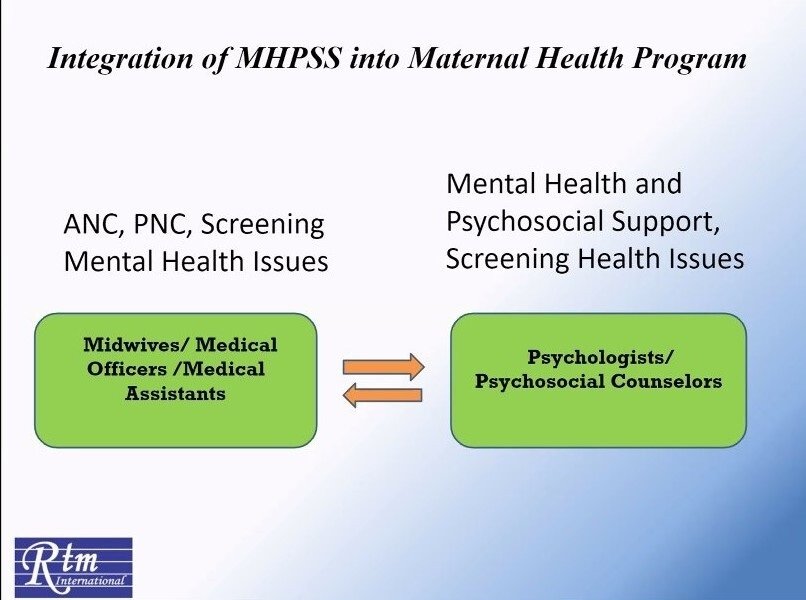
In the second session, speakers (Andrea Barrios – Save the Children, Salma Akhter – RTM International, and Sanni Bundgaard – IRC) presented on three different approaches to delivering integrated MNH care. One example was Save the Children Colombia’s referral pathway approach where upon identification, women are immediately provided with Mental Health and Psychosocial Support (MHPSS) from a social worker and psychologists while simultaneously receiving clinical support from an auxiliary nurse, a general physician, and a gynecologist. Due to the high risk of femicide in Colombia, clients are often also referred to a secure shelter and can qualify for financial assistance. This referral system protects both the physical and mental health of the mother and baby though coordination across various actors from shelter, safety, food, case management, MHPSS, clinical management, and protection.
Additional reflections from IRC and RTM International focused on women and girl safe spaces and the benefits these spaces offer as places to incorporate maternal mental health services and to overall improve wellbeing:
- In Cox’s Bazar, RTM International utilizes Integrated Women Centers to address women’s general and maternal health, gender-based violence (GBV) prevention, and MHPSS in an integrated way, allowing women to receive services, consult with healthcare workers, and participate in activities to improve their overall wellbeing.
- Similarly, IRC has seen a positive impact on the psychosocial well-being of women and girls with the introduction and continuation of these spaces. Sustainability was emphasized as an additional benefit, “If we understand the clients, the safe spaces will become interventions on their own without needing to be attached to a specific organization.6
These approaches aligned with a consistent theme noted throughout the consultation, and especially important to consider in fragile and crisis-affected settings: the need for a continuum of care approach for mental health. As Dr. Laura Murray mentioned on the first day, “It is very rare for a person, especially a person in a fragile or conflict setting, to come forward with just one problem. Instead, they often have multiple needs that must be addressed.” We cannot focus only on maternal mental health during the perinatal period, but instead must consider the entire lifespan of a women’s mental health and wellbeing. We must also examine the relationship between perinatal mental health and children’s mental health. The recently released State of the World’s Children Report recognizes the impact of humanitarian crises on children’s and young people’s mental health, but the linkage between perinatal mental health and children’s mental health is absent. This is a prime moment for the maternal health, child health, and MHPSS communities to collaborate on improved mental health outcomes for mothers and their children in humanitarian settings
It is apparent from this vibrant and in-depth consultation that humanitarian MNH actors are poised to take forward this momentum and explore how best to improve MNH outcomes in crises settings, in partnership with the mental health community. The consultation ended with a call for unity across the humanitarian-development nexus in order to progress maternal mental health forward. Speakers urged participants to focus on incorporating mental health services and support into pre-existing maternal health guidelines, tools, and trainings. Jointly updating global guidance and standards in order to improve maternal mental health through integrated approaches is an opportunity for collaboration between the humanitarian and MHPSS communities.
The need is clear. Mothers in fragile and crises-affected settings are lacking the necessary mental health support they and their families need. Now is the time for the humanitarian community to leverage the momentum from this event. In your work, learn from mothers about their mental health needs, reach out to your MHPSS colleagues and peers to identify areas of alignment, and join in the global conversation happening around maternal mental health. One upcoming chance to join in this conversation is on October 14th, The Wilson Center’s Maternal Health Initiative and UNFPA are hosting a conversation entitled: Maternal Mental Health: Providing Care and Support in the Perinatal Period.
This is our chance to ensure women and girls in fragile and crisis-affected contexts are included in the way forward for maternal mental health.
The author would like to thank all organizers, speakers, and panelists from the Maternal Mental Health Consultation. All session recordings from the event are now available on the virtual platform in unedited format. All presentations and related resources, as well as edited session recordings will be uploaded in the coming weeks.
The IAWG Newborn Initiative (INI) was established in 2020 to accelerate global preparedness and response to deliver high quality maternal and newborn health care, and to improve newborn health and well-being in humanitarian and fragile settings. The INI has a mandate to hold the global community accountable to progressing the priorities agreed upon within the multi-sectoral Roadmap to Accelerate Progress for Every Newborn in Humanitarian Settings 2020-2024. It operates through the IAWG MNH working group, and collaborates closely with both the ENAP in Emergencies working group and the Child Health in Emergencies and Humanitarian Settings working group to jointly advance an evidence-based agenda aimed at delivering a continuum of care across the life course.
References
- The Lancet Global Health. Mental health matters. Lancet Glob Heal. 2020;8(11):e1352. Accessed from: https://www.thelancet.com/jour... ↩
- O’Hara MW, Wisner KL. Perinatal mental illness: Definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):3-12. doi:10.1016/j.bpobgyn.2013.09.002 ↩
- USAID and MOMENTUM. The Silent Burden: A Landscape Analysis of Common Perinatal Mental Disorders in Low- and Middle-Income Countries. September 2021. Accessed from: https://usaidmomentum.org/reso... ↩
- Ndogoni, L. Evidence and Gaps for Women in Fragile and Crisis-Affected Contexts. (2021, 7-9 September). Maternal Mental Health Technical Consultation, virtual: https://mmhtechcon.conference.tc/ ↩
- Ibid ↩
- ”Bundgaard, S. Approaches for Integration of Maternal Mental Health Care in Fragile and Crisis-Affected Contexts. (2021, 7-9 September). Maternal Mental Health Technical Consultation, virtual: https://mmhtechcon.conference.tc/ ↩